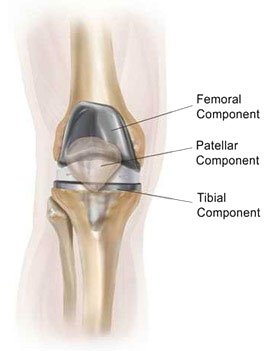
The surface of the femur is replaced with a rounded metal component that comes very close to matching the curve of the natural bone. The surface of the tibia is replaced with a smooth plastic component. A flat metal component holds a smooth plastic piece made of ultra-high-molecular-weight polyethylene plastic that serves as the cartilage. The undersurface of the kneecap may also be replaced with an implant made of the same polyethylene plastic.